| GIS | |
GIS for lymphatic filariasis morbidity management and control
|
M Palaniyandi |
|||||||||||||||
|
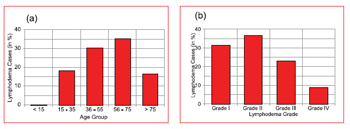
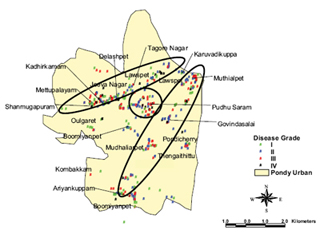
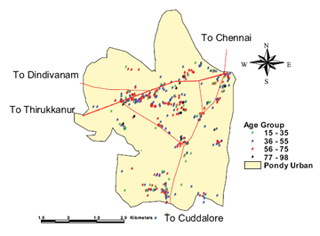
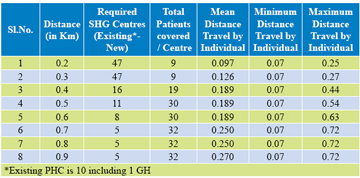
The disability problem due to Lmphatic Filariasis (LF) disease has been reported in 80 countries Ottesan EA (2000). Globally, the 1.1 billion people are exposed to risk of LF and the estimated LF affected population is 120 million Ottesan EA (2000), Michael E et al. (1996). Our recent estimation showed that there are 21 million diseased individuals in India alone Sabesan S et al. (2000) contributing approximately 40 per cent of global burden. A progressive lymphadema with increasing episodic attack adenolymphngistis (ADL) is the most important cause of physical suffering, permanent disability Pani SP and Lall R (1998) and the economic loss of the affected individuals and the community Ramaiah KD et al. (1998, 1999, 2000). Apart from these LF is also responsible for social problems including sexual disability and discomfort of marital life Dreyer G et al (1997). The disease “Lymphatic Filariasis” mainly affect the lymphatic system of a man and it manifest itself in the form of lymphangistis, filarial fever, funiculitis, epididymo-orchitis during acute stages and the chronic phase includes elephantiasis, hydrocele and chronic oedema Pani SP and Lall R (1998). Though the mortality due to filariasis is negligible, regular treatment and management of limb swelling from becoming worse is high degree of attention in view of its disability and disease burden during the entire lifetime of the individual and the community Pani SP and Lall R (1998), Ramaiah KD et al. (1998) and Dreyer G et al (1997). Lymphatic filariasis is recognized as one of the potential eradicable diseases CDC (1993). The Global Alliance for Elimination of Lymphatic Filariasis (GAELF) has recommended that the transmission control and morbidity management are two important pillars in the global elimination strategy for Lymphatic Filariasis (LF) Das PK. and Pani SP (2000). For transmission control, annual single dose mass administration of anti-parasitic drugs Das PK. and Pani SP (2000) is being implemented in several countries including India. The study aimed to provide aids and guidance or a manual massage to diseaseaffected community through self-help groups (SHG) for filariasis morbidity management and control by self-help measures Dreyer G et al (2000), which is recognized as need, based current strategy in the Global Elimination of Lymphatic Filariasis Programme. Materials and Methods Study SiteThe study site, Pondicherry is the capital of Pondicherry Union Territory, which is located in the East coast of South India about 160 Km south of Chennai (formerly Madras), it geographically extends between 11o 53’ 45” N and 11o 58’ 55” N, 79o 46’ 15” E and 79o 50’ 50” E. It has the geographical area measured to 48.06 Sq. Km. Monsoon is experienced from October to December in every year. Total urban population is 516,985, (Males 260,482 and Females 256,503) and the total number of households is 101,481 (Census of India 2001). Study DesignThe study was designed for the selection of appropriate service locations for morbidity management for filariasis disease, mainly considering the patients convenience, using GIS decision support tool. It provides to capture the filariasis disease data in electronic mode and attach the same to the digital map of the study area for the spatial analysis on GIS Platform. The study was carried in three stages. In the initial stage, field data was collected through reconnaissance survey, which was conducted in every doorstep in every street of the study site. In the second stage, a geo-database was created and which was linked to the GIS spatial database engine for depicting the attributes on the digital map of the study site for preparation of distribution map and further spatial analysis. Finally, to develop a decision support tool, spatial analysis was carried out for determining the appropriate locations and allocating optimum patients to each self-help morbidity management centre considering distance and other basic facilities (i.e. roads, transports, electricity, water, accommodations, and SHG). Figure 1. (a) The occurrence of lymphodema cases in different age group, and (b) lymphodema cases with different grade in Pondicherry Urban. The data is pooled into a single GIS platform to achieve the objectives. Mapping the existing health facilities and identifying the new locations for opening self-help health centres in the center of every disease cluster (community) with minimum distance coverage for local treatment, was consider as main factor for the decision support tool. This was based on the understanding of people’s intricacy for traveling long distance i.e. more than half a kilo metre for local treatment and the huge expenditure for periodical traveling for morbidity management are the background key factors of the spatial ring buffering analysis, and thus, the study was framed with a hypothesis that no lymphodema patient would prefer to travel beyond 1 Km distance for seeking treatment. Figure2. Study area of Pondicherry Urban showing the filariasis lymphodema disease with different grades The self-help Health Service CentresThe self-help groups included voluntary organizations, youth club, NGOs, youth welfare association and community movements. The distance of each distance ring buffer was measured from the center of each disease clusters to the peripherals of each lymphodema case household location. Based on the distance and other basic facilities and in the patient’s convenience, the existing PHC, GH in and around the study areas are plotted for optimum allocation of the patients to the existing facilities and identified appropriate new locations for opening Self Help health Centres. Figure 3. Filariasis lymphodema Cases classified in to different age group (based on spatial cluster analysis), major roads (line showing red colour) are overlaid on the urban map Results and DiscussionsTotally, 482 cases (both males and females) were identified and these were recorded properly, using GARMIN GPS 12XL. The preliminary analysis shows that < 15 years we have no record on lymphodema case, working adult age group 15 to 35 years is potentially having problem of 18 per cent, and steadily increased 30.3 per cent in the 35 to 55 years age group (working middle age group), in the later age group of > 55 to 75 years having record of 35.3 per cent (170 cases), and finally, 16.4 per cent (79 cases) were recorded in the age group of < 75 years. It shows that the potential working age group is affected severely. In the over all view, grade II is highest record of 36.7 per cent and followed by grade-I 31.2 per cent, grade III 23.2 percent and grade IV 8.9 per cent are recorded. Disease time duration of having lymphodema problem is assessed by questionnaire method. Based on this questionnaire, 228 (47%) cases were identified with disease for the past 1 year, 108 (22%) cases were assessed having problem of disease for 1-10 years, 73 (15.1%) cases were recorded with disease problem for 10-20 years, 20 (4.1%) cases were having disease problem for the period of 20 to 30 years and finally, the disease cases recorded to 53 (10.9%) with more than 30 years (Fig.1a and 1b). Required number of SHGC with different distant rule for optimum allocation of patients to each SHGC for filariasis morbidity management: The Digital map of Pondicherry urban was prepared Map Info 4.5 GIS platform. The digital data was captured in to GIS platform for plotting the locations of the disease cases. These disease cases were further classified with filariasis lymphodema grade wise and age wise distribution (fig2. and fig.3). Selection of self-help Health Service centresSpatial ring buffering, spatial clustering, and nearest neighbourhood analysis was performed for easy understanding of spatial pattern and disease clustering. The distributions of the disease cases are found two major linear patterns and one ring cluster (fig.2). Though the lymphodema cases proportionally high in the 56 -75 years of age group and the presents of lymphodema grade II cases is high in percentage it has found in all over the human settlements (fig.3). The list of existing PHC/ GH is depicted on the Pondicherry urban boundary map. The different distance rule of 0.2KM, 0.3KM, 0.4KM 0.5 KM, 0.6, 0.7 KM, 0.8 and 0.9 KM were created over the disease distribution map, using spatial ring buffering technique at GIS platform. The minimum, maximum and the mean distances of each disease cluster are calculated against to each distance rule/ ring buffering. Since, the K-mean patients density 1.89 Km, the spatial ring buffering performance started from 0.2KM, and it is increased by 0.1KM and which is extended up to 1KM. Figure 4. Optimum allocation of patients to the existing health centres and the proposed new location for opening SHG health centres: rule fixed 0.4 Km ring buffer only Number of existing centers and the required centers against each distance rule (0.2KM, 0.3KM, 0.4KM, 0.5KM, 0.6KM, 0.7Km, 0.8KM, 0.9Km & 1.0KM) were calculated and tabulated for the optimum coverage of the patients with in the specified distance coverage. Ring buffering of 0.2KM, 0.3Km and 0.4Km are overlaid on lymphodema distribution map and derived the output of 0.4 Km ring buffer (Fig.4). The results of 0.5Km and 0.6Km ring buffers are giving the same results of 0.4Km distance ring buffer, therefore, next analysis, the distance of 0.7Km, 0.8Km, and 0.9Km ring buffers are overlaid on lymphodema cases and obtained 0.7Km as the output of second analysis (Fig.5). ConclusionThe distributions of the disease cases are found to be linear pattern of spatial distribution associated with major roads system. The lymphodema cases proportionally high in the 56 -75 years of age group and the presents of lymphodema grade II and lymphodema grade III cases are high in percentage. The study gives result that with 0.7 KM ring buffering distance is having optimum service coverage. The present study hypothesis is that the aged patients could travel less than 1KM distance from their residence to the health centres for morbidity management is care fully examined. The study area required 15 centres with 0.7KM distance ring buffer or coverage area, out of 15, 10 centres are already existed, and 5 more new centres only required covering all the patients. We suggest that opening self-help health service centres with coverage of less than 1-kilometer distance in urban like Pondicherry is ideal. Figure 5 Optimum allocations of patients to the existing health centres and the proposed new location for opening SHG health centres: rule fixed by 0.7Km, ring buffer only AcknowledgementThe author is grateful to the Director, Vector Control Research Centre, Puducherry- 60506, India, for permitting to carryout this study, providing facilities and clinical staff support for collecting data. ReferencesCDC 1993 “Recommendation of the International Task force for Disease Eradication; Morbidity and Mortality”,. Weekly Report, 42: 1-38. # Das PK., Pani SP 2000 “Towards elimination of lymphatic filariasis in India: Problems, Challenges, Opportunities and new initiatives”, JIMSA Jan-Mar., 13 (1): 18-26 # Dreyer G., Noraes J, Addiss D Figure 4. Optimum allocation of patients to the existing health centres and the proposed new location for opening SHG health centres: rule fixed 0.4 Km ring buffer only 1997 “The Silent burden of sexual disability associated with lymphatic filariasis”, Acta Tropica, 63: 57-60 # Dreyer G, Addiss D, Bettingr J, Dreyer P, Noroes J, Rio F 2000 “Introduction. Lymphoedema Self Manual”, Treatment and Prevention of problems associated lymphatic filariasis, WHO, Geneva, V-VII # Michael E, Bundy DAP, Grenfell BT 1996 “Re-assessing the global prevalence and distribution of lymphatic filariasis”, Parasitology, 112: 409-428 # Ottesan EA 2000 “The global programme to eliminate lymphatic filariasis”, Trop Medicine & International Health, 5: 591-594 # PaniSP, Lall R 1998 “Clinical features, Pathogenesis and Management of Lymphatic Filariasis”, Indian Council of Medical Research (ICMR) Bulletin, 28: 41-51 # Pondicherry Census Gazette: Census of India 2001 # Ramaiah KD, Ramu K, Guyatt H, Vijaya Kumar KN, Pani SP 1998 “Direct and indirect cost of the acute form of lymphatic filariasis to house holds in rural areas of Tamil Nadu, South India”, Tropical Medicine and International Health, 3: 108-115 # Ramaiah KD, Guyatt H, Ramu K, Vanamail P, Pani SP, Das PK 1999 “Treatment cost and loss of work time to individuals with chronic lymphatic filariasis in rural communities in South India”, Tropical Medicine and International Health, 4 (1): 19-25 # Ramaiah KD, Das PK, Michael E, Guyatt H 2000 “The economic burden of lymphatic fiariasis in India”, Parasitology Today, 16: 251-253 # Sabesan S, Palaniyandi M, Edwin M, Das P K 2000 “Mapping of Lymphatic Filariasis at the district level in India”, Ann. Trop. Med. & Para, 94 (6): 591-606 |
|||||||||||||||
|
|||||||||||||||
|














 (No Ratings Yet)
(No Ratings Yet)